Until the 90’s, males with very low counts (less than 5 million per ml) or poor quality sperms had no hope of fathering their own genetic children. This problem was triumphed by the new breakthrough of ICSI.
In our partner facility, ICSI as a treatment was offered since 1998-99 and till date more than 10,000 cycles with success rate of 40 to 50% per cycle have been performed.
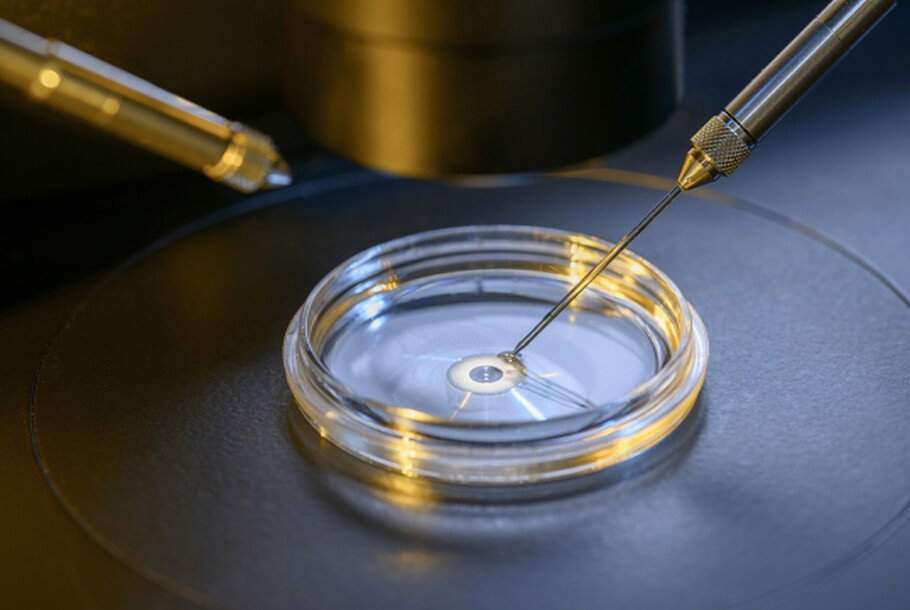
In ICSI, all the steps are similar to the procedure of IVF, except the step of fertilization.Normally in IVF, one egg is mixed with 200,000 sperms and one of the sperms fertilizes the egg on its own. In contrast, in ICSI, each egg is held and injected with a single live sperm.